Human Microbiome and Normal Flora of Human Body
In this enlightening video, we delve into the fascinating world of the human microbiome and the normal flora that inhabit our bodies. Discover how these microorganisms play a crucial role in maintaining our health, influencing everything from digestion to immune function. We will explore the diverse ecosystems found in various body sites, including the gut, skin, and oral cavity, and discuss the implications of microbiome imbalances on human health. Join us as we uncover the intricate relationships between humans and their microbial companions, and learn how to support a healthy microbiome for overall well-being. #HumanMicrobiome #NormalFlora #GutHealth
Website: https://biologynotesonline.com/
Facebook: https://www.facebook.com/biologynotesonline
Instagram: https://www.instagram.com/biologynotesonline/?hl=en
human microbiome,microbiome,normal flora,gut microbiome,normal flora of human body in microbiology,normal microbial flora,normal flora of human body,human gut microbiome,normal flora of the human body,normal flora of skin,what is normal flora of human body,what is normal microbiota of human body,how normal flora establish in human body?,human oral microbiome,human microbiota,normal body flora,normal bacterial of human,human microbial flora
Show More Show Less View Video Transcript
0:00
the human microbiome is the collection
0:02
of trillions of microorganisms living on
0:04
and inside the human body the microbiome
0:08
includes various types of microorganisms
0:11
bacteria are the most numerous but fungi
0:13
viruses and other microbes also play
0:16
important
0:17
roles these microorganisms are mostly
0:20
beneficial and essential for human
0:22
health they aid in digestion and
0:24
nutrient absorption train our immune
0:26
system and protect us from harmful
0:28
pathogens
0:30
the scale of the microbiome is
0:32
impressive microbial cells outnumber
0:34
human cells by a ratio of about 10:1
0:37
together they weigh about 2 kg roughly
0:40
the weight of a human
0:42
brain the microbiome is distributed
0:45
throughout the body with distinct
0:47
communities in different locations the
0:49
skin hosts a diverse community adapted
0:52
to different environmental conditions
0:54
the oral cavity and respiratory tract
0:56
have their own unique populations the
0:59
gut contains the largest and most
1:01
diverse microbial community the
1:03
eurogenital tract maintains specialized
1:06
microorganisms adapted to its unique
1:11
environment our body hosts two main
1:14
types of normal flora resident and
1:17
transient normal flora are
1:19
microorganisms that inhabit our body
1:21
surfaces without causing disease under
1:23
normal conditions
1:27
let's compare the two main types of
1:29
flora that live on and in our bodies
1:31
resident flora are permanent inhabitants
1:33
of the body while transient flora are
1:36
temporary visitors resident flora are
1:38
permanent inhabitants that have
1:40
established themselves in specific body
1:42
locations they are well adapted to their
1:45
environments and maintain stable
1:46
populations
1:48
transient flora in contrast are
1:50
temporary visitors that may be present
1:52
for hours days or weeks before being
1:55
removed their populations fluctuate
1:58
significantly resident flora provide
2:00
long-term benefits like preventing
2:02
pathogen colonization and supporting
2:04
immune function transient flora may be
2:07
beneficial neutral or potentially
2:08
harmful depending on circumstances
2:12
let's look at some examples of where we
2:14
find resident and transient flora in the
2:17
human body resident flora include
2:19
stafyloccus epidermis on the skin
2:21
lactobacillus in the gut and
2:23
streptococcus in the mouth transient
2:26
flora may include ecoli temporarily on
2:28
hands seasonal respiratory microbes and
2:31
food associated bacteria passing through
2:33
the
2:35
gut both resident and transient flora
2:38
play important roles in our health
2:39
resident flora provide colonization
2:42
resistance by occupying niches that
2:44
might otherwise be filled by pathogens
2:47
they also help train our immune system
2:49
from birth transient flora introduce
2:52
microbial diversity and can bring new
2:54
beneficial functions like additional
2:56
digestive capabilities the balance
2:58
between both types is key to maintaining
3:01
health
3:04
the human skin is home to diverse
3:06
microbial communities that play crucial
3:08
roles in maintaining skin health
3:11
different skin regions harbor distinct
3:13
microbial populations based on the local
3:16
environment conditions the composition
3:18
of skin microbiota is influenced by
3:20
several factors including moisture
3:22
levels pH sebum production and
3:25
temperature let's take a closer look at
3:27
the key bacterial species that dominate
3:29
the skin microbiome stafylocus epidermis
3:33
is the most abundant bacterium on the
3:35
skin surface playing a crucial role in
3:38
maintaining skin health corina bacteria
3:40
thrive in moist areas such as the armpit
3:43
and groin contributing to body odor
3:45
through their metabolic activities
3:47
propionabacteria dominate sebaceous
3:49
regions like the face and scalp where
3:51
they break down sebum into free fatty
3:53
acids that help maintain skin pH the
3:56
skin microbiome serves several important
3:59
functions that benefit our skin and
4:01
overall health let's examine a
4:03
cross-section of skin to better
4:05
understand where different microbial
4:07
communities
4:10
reside these microbes interact with skin
4:13
cells in various ways forming a complex
4:15
ecosystem understanding the skin
4:17
microbiome helps us appreciate how these
4:20
microbial communities contribute to skin
4:22
health and immunity section four oral
4:26
and respiratory microbiomes the human
4:28
body hosts complex microbial communities
4:30
in both the oral cavity and respiratory
4:33
tract the oral microbiome is one of the
4:35
most diverse microbial communities in
4:37
the human body containing hundreds of
4:39
bacterial species that form complex
4:42
ecosystems key species include
4:44
streptococcus mutants which forms dental
4:47
plaque and pframonus which is associated
4:49
with gum disease
4:51
these and other bacteria have adapted to
4:54
specific niches within the mouth these
4:56
bacteria form dental bofilms through a
4:58
multi-stage process first bacteria
5:00
attach to the tooth surface then they
5:03
multiply to form microcolonies finally a
5:06
mature bofilm develops with a protective
5:08
matrix that shields the bacteria in
5:10
contrast to the oral cavity the
5:12
respiratory tract shows a gradient of
5:14
microbial colonization the upper
5:16
respiratory tract including the nasal
5:18
passages and throat contains various
5:21
microbes however the lower respiratory
5:24
tract is nearly sterile in healthy
5:26
individuals with only minimal microbial
5:28
presence throughout both the oral cavity
5:30
and respiratory tract microbes interact
5:33
with mucous membranes these microbes
5:36
colonize the mucous layer covering
5:38
epithelial cells forming a protective
5:40
barrier and interacting with the host
5:42
immune system one of the most important
5:44
functions of the normal flora in these
5:46
regions is preventing infection through
5:49
competitive exclusion resident microbes
5:51
occupy attachment sites produce
5:53
antimicrobial substances and compete for
5:56
nutrients thereby preventing
5:58
colonization by respiratory
6:01
pathogens the balance of microbes in the
6:03
oral and respiratory microbiomes is
6:06
crucial for health disruption of these
6:08
communities can lead to conditions like
6:10
dental carries periodontal disease or
6:12
respiratory
6:16
infections let's explore the gut
6:18
microbiome and the differences between
6:20
the small and large
6:22
intestines the gut microbiome varies
6:25
dramatically throughout the digestive
6:26
tract with a gradient of microbial
6:29
populations from the stomach to the
6:30
colon
6:33
the small intestine has relatively few
6:35
microbes due to rapid transit time and
6:37
antimicrobial secretions like bile
6:40
bacterial density here ranges from 10
6:42
quip to 10 fret colony forming units per
6:44
milliliter predominantly firmicutes and
6:47
proteobacteria filyla the environment is
6:50
less hospitable to microbes due to rapid
6:52
transit time and antimicrobial bile
6:54
salts and digestive enzymes
6:57
this area focuses on nutrient absorption
7:00
rather than microbial
7:02
fermentation in contrast the large
7:04
intestine contains the highest microbial
7:07
density in the human body bacterial
7:09
counts reach an astounding 10 to 10
7:12
squared colony forming units per
7:14
milliliter primarily dominated by
7:16
firmicutes and bactaroides fila these
7:19
large intestinal microbes perform
7:21
critical functions like breaking down
7:23
complex carbohydrates that our digestive
7:25
enzymes cannot
7:27
process through fermentation they
7:29
produce short-chain fatty acids like
7:31
butyrate acetate and propionate which
7:34
nourish intestinal cells and regulate
7:36
metabolism these gut microbes
7:38
continuously interact with intestinal
7:40
cells influencing immune function and
7:43
maintaining the intestinal barrier
7:47
we can observe a clear gradient of
7:49
microbial populations as we move from
7:51
the stomach through the small intestine
7:53
and into the large
7:55
intestine bacterial density increases
7:58
dramatically from approximately 10 to 10
8:00
wqui in the stomach reaching 10 to 10
8:03
fights in the terminal illium and
8:05
culminating at 1011 to 101 quoid in the
8:08
colon
8:10
to summarize the key differences the
8:12
small intestine has fewer microbes
8:15
different dominant bacterial filyla and
8:17
focuses on nutrient absorption the large
8:20
intestine has much higher bacterial
8:22
density longer transit time and
8:24
specializes in fermentation of complex
8:27
carbohydrates producing beneficial
8:29
metabolites for the host
8:33
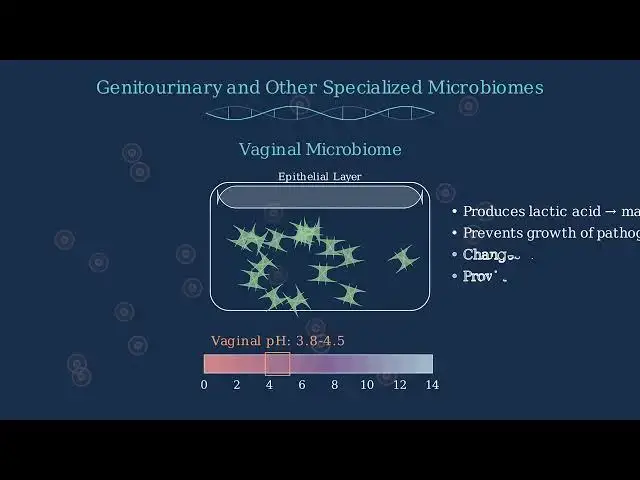
specialized microbiomes exist throughout
8:35
the body adapting to unique local
8:38
environments and providing tailored
8:40
protection the vaginal microbiome is
8:42
predominantly composed of lactobacillus
8:44
species these beneficial bacteria are
8:46
critical for maintaining vaginal
8:49
health lactobacilli produce lactic acid
8:52
which maintains the vaginal pH between
8:54
3.8 and 4.5 this acidic environment
8:57
prevents the growth of pathogenic
8:59
bacteria the vaginal microbiome
9:01
composition changes during the menstrual
9:03
cycle and pregnancy but consistently
9:06
provides a crucial barrier against
9:09
infections unlike most body sites the
9:12
urinary tract is typically sterile above
9:14
the urethra meaning it normally contains
9:17
no microorganisms the sterility is
9:19
maintained by regular urine flow which
9:21
flushes away potential pathogens only
9:24
the urethal entrance may harbor some
9:26
resident microbes this is a stark
9:29
contrast to the vaginal microbiome which
9:31
has a high bacterial load and acidic pH
9:33
while the urinary tract has very few
9:35
microbes and a more neutral
9:38
pH the ear canal supports a sparse but
9:41
specialized microbiome unlike internal
9:44
ear structures which are typically
9:46
sterile the ear canal harbors a small
9:48
community of microorganisms
9:50
this microbiome is primarily dominated
9:52
by stafylocus and coronabacterium
9:55
species camin commonly known as ear wax
9:58
contains antimicrobial compounds that
10:00
help regulate the microbial population
10:03
and maintain ear canal health the
10:06
conjunctiva of the eye supports an
10:08
extremely sparse microbiome this
10:10
environment is continuously cleared by
10:12
blinking which mechanically removes
10:15
microorganisms the tier film contains
10:17
powerful antimicrobial compounds like
10:19
lysosyme which destroys bacterial cell
10:22
walls and lactopherin which sequesters
10:24
iron needed for bacterial growth these
10:27
adaptations keep the eye surface nearly
10:30
sterile each specialized microbiome has
10:33
evolved unique adaptations to its local
10:35
environment the vaginal microbiome
10:38
maintains an acidic pH through
10:40
lactobacillus activity the urinary tract
10:43
remains nearly sterile due to regular
10:45
urine flow the ear canal is protected by
10:48
antimicrobial compounds in serumin and
10:50
the eye conjunctiva is defended by
10:52
powerful enzymes in tears these
10:54
microbiomes have evolved specific
10:56
defense mechanisms adapted to their
10:58
unique anatomical locations and
11:00
physiological
11:03
conditions various factors shape the
11:05
composition of our microbiome impacting
11:07
which organisms thrive and which decline
11:10
age affects which microbes populate our
11:13
bodies from birth through adulthood to
11:14
old age diet has one of the strongest
11:17
impacts especially on gut microbiome
11:20
composition hormonal changes during
11:22
puberty pregnancy and menopause alter
11:24
microbial communities hygiene practices
11:27
like handwashing and bathing influence
11:29
skin and mucosal microbiomes antibiotic
11:32
use can dramatically disrupt normal
11:34
microbial balance often with lasting
11:37
effects immune system status determines
11:39
which microbes are tolerated versus
11:41
eliminated environmental exposures
11:44
including location animals and plants
11:46
introduce new microbes genetic factors
11:49
influence which microbes can establish
11:51
themselves in our bodies let's take a
11:53
closer look at how diet impacts our
11:56
microbiome diet has a particularly
11:58
strong influence on gut microbiome
12:00
composition with different food groups
12:02
promoting different bacterial
12:04
communities
12:05
a diet rich in plant fibers promotes
12:08
beneficial bacteria like bactaroides and
12:11
bifidobacteria while high protein diets
12:13
favor different communities like
12:15
proteobacteria our microbiome also
12:17
changes throughout our lifetime our
12:19
microbiome evolves throughout our
12:21
lifespan beginning at birth and
12:23
continuing to change as we age newborns
12:26
start with limited microbial diversity
12:28
which rapidly increases during infancy
12:30
and childhood diversity peaks in
12:32
adulthood before decreasing in old age
12:35
antibiotics can dramatically disrupt our
12:38
microbiome balance before antibiotic
12:40
treatment our microbiome exists in a
12:43
balanced state with diverse beneficial
12:45
bacteria during antibiotic treatment
12:47
both harmful and beneficial bacteria are
12:50
significantly reduced in the recovery
12:52
phase bacteria begin to repopulate but
12:55
the balance may be temporarily disrupted
12:58
eventually a new equilibrium is
13:00
established though it may differ from
13:02
the original microbiome composition
13:04
multiple factors continuously shape our
13:07
microbiome throughout life from diet and
13:10
age to antibiotics and genetics creating
13:12
our unique microbial
13:14
fingerprint understanding these
13:16
influences helps us maintain and restore
13:19
microbiome health normal flora the
13:21
microorganisms that typically inhabit
13:23
our bodies can become harmful under
13:26
certain conditions
13:27
these are called opportunistic pathogens
13:30
normally harmless microbes that take
13:32
advantage of opportunities to cause
13:35
disease one way normal flora becomes
13:38
harmful is by entering the wrong body
13:40
location a classic example is urinary
13:42
tract infections echericia or E.coli
13:46
normally lives harmlessly in our
13:47
intestines but if these bacteria
13:50
transllocate to the urinary tract they
13:52
can cause infection and inflammation
13:55
another way normal flora becomes harmful
13:57
is when host defenses are compromised in
14:00
the oral cavity we normally maintain a
14:02
balanced microbial community when
14:05
factors like high sugar diet poor oral
14:07
hygiene or reduced saliva flow
14:09
compromise our defenses bacteria like
14:12
streptoccus mutants can overgrow and
14:14
cause dental
14:16
carries this shift from healthy
14:18
microbiome to disease-causing state is
14:20
called disbiosis a microbial imbalance
14:23
that contributes to various diseases in
14:26
a balanced microbiome beneficial and
14:28
commensal bacteria dominate with
14:30
potential pathogens kept in check
14:32
various triggers like antibiotics diet
14:35
changes inflammation or stress can
14:37
disrupt this balance leading to
14:39
disbiosis where potential pathogens
14:42
overgrow one of the most dramatic
14:44
examples of normal flora becoming
14:46
harmful is claustrdium diffosil
14:48
infection in a healthy gut a diverse
14:51
microbiome keeps potential pathogens
14:53
like ced difficil in check through
14:55
competition antibiotic treatment while
14:58
targeting pathogens also eliminates
15:00
beneficial bacteria that normally
15:02
compete with
15:03
cedicil this creates an opportunity for
15:06
seed difficil to multiply rapidly
15:08
causing severe diarrhea inflammation and
15:11
potentially life-threatening
15:14
complications maintaining a healthy
15:16
microbiome is crucial for overall health
15:20
probiotics are live microorganisms that
15:22
provide health benefits when consumed in
15:25
adequate amounts they help restore and
15:27
maintain beneficial bacteria in the gut
15:30
common sources of probiotics include
15:32
yogurt kimchi kefir and
15:34
kombucha prebiotics are specialized
15:37
plant fibers that act as food for
15:39
beneficial bacteria unlike probiotics
15:42
prebiotics aren't living organisms but
15:44
rather nutrients that help existing good
15:47
bacteria thrive when prebiotic fiber
15:49
reaches the gut it serves as nourishment
15:51
for beneficial bacteria helping them
15:53
multiply and produce helpful compounds
15:56
prebiotic foods include garlic onions
15:58
bananas oats apples and flax
16:01
seeds fecal microbiota transplantation
16:04
or FMT is a procedure that transfers
16:06
fecal bacteria from a healthy donor to
16:09
restore the gut microbiome of a
16:11
recipient the process involves
16:12
collecting stool from a carefully
16:14
screened healthy donor processing it in
16:17
a laboratory and then delivering it to
16:19
the recipient through various methods
16:21
such as colonoscopy enema or capsules
16:25
fmt is primarily used to treat recurrent
16:27
claustrdium diffosil infections with
16:30
success rates of around 90% after one or
16:33
two
16:34
treatments there are several practical
16:36
ways to maintain a healthy microbiome in
16:39
everyday life eating a diverse
16:41
plant-based diet rich in fiber provides
16:43
fuel for beneficial bacteria limiting
16:46
unnecessary antibiotic use helps
16:49
preserve your existing microbial
16:51
communities regular physical activity
16:53
has been shown to increase microbial
16:55
diversity managing stress is important
16:58
as stress hormones can alter gut
17:00
bacteria composition quality sleep is
17:02
also essential as disrupted sleep
17:04
patterns can negatively impact the
17:06
microbiome
17:08
looking to the future scientists are
17:10
developing targeted microbiome based
17:13
therapies for various health conditions
17:16
for inflammatory bowel disease
17:17
microbiome based treatments show
17:19
significant promise with clinical trials
17:22
already underway research on addressing
17:24
obesity and metabolic disorders through
17:26
microbiome manipulation is progressing
17:29
rapidly the gutbrain axis connection has
17:32
opened new avenues for treating mental
17:34
health conditions through the
17:36
microbiome early research suggests the
17:39
microbiome may also influence cancer
17:41
treatment responses particularly in
17:43
immunotherapy maintaining microbiome
17:46
health requires both preventive measures
17:48
and targeted interventions as research
17:51
advances personalized microbiome
17:53
approaches may become standard in
17:55
healthcare
#Hygiene & Toiletries
#Health Conditions
#Infectious Diseases